Achalasia Cardia
Achalasia Cardia is a rare disorder that makes difficult for food and liquid to pass through esophagus into your stomach. The act of swallowing causes a wave of esophageal contraction called peristalsis. Peristalsis pushes food along the esophagus and there coordinated relaxation of lower esophageal sphincter. In achalasia, lower esophageal sphincter fail to relaxation on swallow i.e. ❝failure to relax❞ and the esophageal sphincter remains contracted. Normal peristalsis is interrupted and food cannot enter the stomach.
Dysphagia, or difficulty swallowing, is the most common symptom of achalasia. Diagnosis begins with a careful medical history. Endoscopy is used to look directly at the surface of the esophagus and Gastro-esophageal junction. This test can also detect tumors that cause symptoms like those of achalasia. Esophageal Manometry confirm diagnosis of Achalasia.
Pneumatic Balloon dilatation for achalasia can be safely undertaken as an outpatient procedure in most patients.
The patient must be fasted, and in the setting of achalasia this often requires a more extended period without solid food to avoid performing a procedure on a patient with a very large volume of esophageal food debris, which is tedious to clear and increases the risk of peri-procedural aspiration. Balloon dilatation done under day care anesthesia.
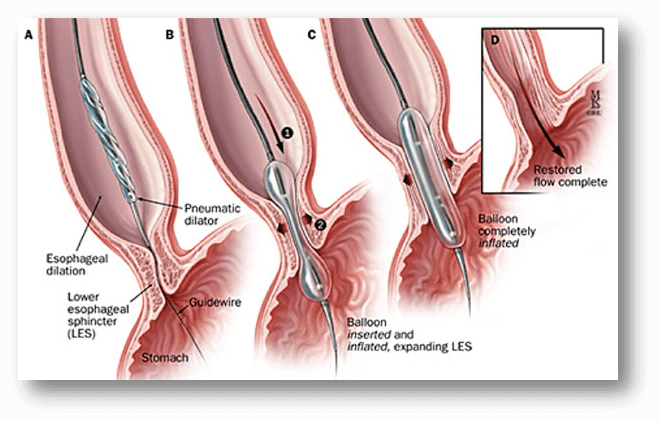
Once the patient is anesthetized, standard endoscopy is performed. Thorough lavage of any esophageal liquid and food residue should be performed to aid in assessment of the esophagus and decrease the risk of substantial meditational contamination if perforation occurs. The gastro-esophageal junction is thoroughly inspected to assess the degree of spontaneous relaxation (if any) and rule out any other potential cause for esophago-gastric outflow obstructions (i.e., pseudo-achalasia).
A Rigiflex™ Balloon (Boston Scientific, MA) is then inserted over the guide wire and passed under fluoroscopic guidance until centered over the gastro-esophageal junction. Under fluoro radio-opaque markers in the balloon used to ensure accurate positioning.
The balloon is fully inflated via a hand held manometer and a waist in the middle of the balloon at the level of the gastro-esophageal junction can be appreciated, and observed to efface as the balloon effectively dilates the lower esophageal sphincter. The balloon is then withdrawn. A check endoscopy is then performed in order to assess the degree of trauma at the gastro-esophageal junction. There should be some mucosal trauma at GE junction. Oral intake can be started when patient sufficiently awake, and discharged within a few hours.
Other treatments options are medications, Heller’s myotomy, Peroral Endoscope Myotomy (POEM).